Dostęp do tego artykułu jest płatny.
Zapraszamy do zakupu!
Po dokonaniu zakupu artykuł w postaci pliku PDF prześlemy bezpośrednio pod twój adres e-mail.
MS 2019; 10: 8-51.
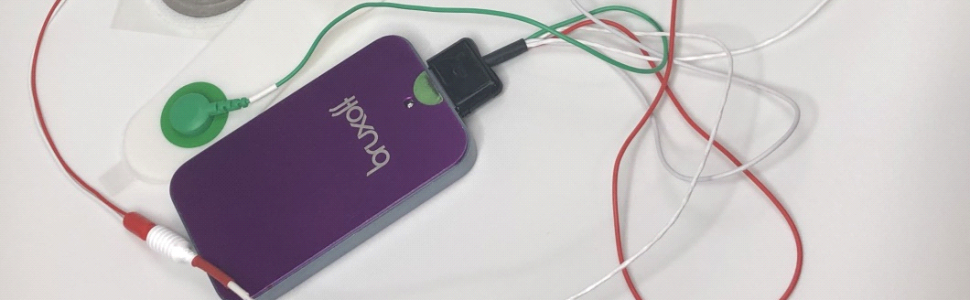
Hasła indeksowe: elektromiografia, bruksizm nocny, Bruxoff, przegląd piśmiennictwa
Key words: electromyography, sleep bruxism, Bruxoff, literature review
PIŚMIENNICTWO
- Okeson J.P.: Leczenie dysfunkcji skroniowo-żuchwowych i zaburzeń zwarcia. Wydawnictwo Czelej, Lublin 2018, 124-130.
- De Leeuw R.: Orofacial pain. Guidelines for assessment, diagnosis and management. 6th edition. Quintessence, Chicago 2018, 146, 229, 243.
- Lobezzo F. i wsp.: Bruxism defined and graded: An international consensus. J. Oral Rehabil., 2013, 40, 2-4.
- Rompre P.H. i wsp.: Identification of a sleep bruxism subgroup with a higher risk of pain. J. Dent. Res., 2007, 86, 837-842.
- Ella B. i wsp.: Bruxism in movement disorders: A comprehensive review. J. Prosthodont., 2017, 26, 599-605.
- Ram S. i wsp.: Using oral medications, infusions and injections for differential diagnosis of orofacial pain. J. Calif. Dent. Assoc., 2006, 34, 645-654.
- Lavigne G.J. i wsp.: Bruxism physiology and pathology: An overview for clinicians. J. Oral Rehabil. 2008, 35, 476-494.
- Lavigne G.J., Montplaisir J.Y.: Restless legs syndrome and sleep bruxism: Prevalence and association among Canadians. Sleep, 1994, 17, 739-743.
- Ohayon M.M., Li K.K., Guilleminault C.: Risk factors for sleep bruxism in the general population. Chest, 2001, 119, 53-61.
- Laberge L. i wsp.: Development of parasomnias from childhood to early adolescence. Pediatrics, 2000, 106, 67-74.
- Ng D.K. i wsp.: Prevalence of sleep problems in Hong Kong primary school children: A community-based telephone survey. Chest, 2005, 128, 1315-1323.
- Lavigne G.L. i wsp.: Cigarette smoking as a risk factor or an exacerbating factor for restless legs syndrome and sleep bruxism. Sleep, 1997, 20, 290-293.
- Hojo A. i wsp.: Association between the amount of alcohol intake and masseter muscle activity levels recorded during sleep in healthy young women. Int J. Prosthodont., 2007, 20, 251-255.
- Winocur E. i wsp.: Drugs and bruxism: A critical review. J. Orofac. Pain, 2003, 17, 99-111.
- Saito M. i wsp.: Temporal association between sleep apnea-hypopnea and sleep bruxism events [epub ahead of print 4 Nov 2013]. J. Sleep Res. doi: 10.1111/jsr.12099
- Manfredini D. i wsp..: Anxiety symptoms in clinically diagnosed bruxers. J. Oral Rehabil., 2005, 32, 584-588.
- Pingitore G., Chrobak V., Petrie J.: The social and psychologic factors of bruxism. J. Prosthet. Dent., 1991, 65, 443-446.
- Kato T., Lavigne G.J.: Sleep bruxism: A sleep-related movement disorder. Sleep Med. Clin., 2010, 5, 9-35.
- Macaluso G.M. i wsp.: Sleep bruxism is a disorder related to periodic arousals during sleep. J. Dent. Res., 1998, 77, 565-573.
- Kydd W.L., Daly C.: Duration of nocturnal tooth contacts during bruxing. J. Prosthet. Dent., 1985, 53, 5, 717-721.
- Reding G.R. i wsp.: Nocturnal teeth-grinding: all-night psychophysiologic studies. J. Dent. Res., 1968, 47, 5, 786-797.
- Clarke N.G., Townsend G.C.: Distribution of nocturnal bruxing patterns in man. J. Oral Rehabil., 1984, 11, 6, 529-534.
- Trenouth M.J.: The relationship between bruxism and temporomandibular joint dysfunction as shown by computer analysis of nocturnal tooth contact patterns. J. Oral Rehabil., 1979, 6, 1, 81-87.
- Clarke N.G., Townsend G.C., Carey S.E.: Bruxing patterns in man during sleep. J. Oral Rehabil., 1984, 11, 2, 123-127.
- Rugh J.D.: Feasibility of a laboratory model of nocturnal bruxism. J. Dent. Res., 1991, 70 (special issue), 554.
- Christensen L.V., Mohamed S.E.: Contractile activity of the masseter muscle in experimental clenching and grinding of the teeth in man. J. Oral Rehabil., 1984, 11, 2, 191-199.
- Christensen L.V.: Facial pain and internal pressure of masseter muscle in experimental bruxism in man. Arch. Oral Biol., 1971, 16, 9, 1021-1031.
- Christensen L.V., Mohamed S.E., Harrison J.D.: Delayed onset of masseter muscle pain in experimental tooth clenching. J. Prosthet. Dent., 1982, 48, 5, 579-584.
- Christensen L.V.: Facial pain from experimental tooth clenching. Tandlaegebladet, 1970, 74, 2, 175-182.
- Christensen L.V.: Some subjective-experiential parameters in experimental tooth clenching in man. J. Oral Rehabil., 1979, 6, 2, 119-136.
- Dutra K.M. i wsp.: Orofacial activities in sleep bruxism patients and in normal subjects: a controlled polygraphic and audio-video study. J. Oral Rehabil., 2009, 36, 2, 86-92.
- Marbach J. i wsp.: The validity of tooth grinding measures: etiology of pain dysfunction syndrome revisited. J. Am. Dent. Assoc., 1990, 120, 3, 327-333.
- http://www.bruxoff.com
- Mayer G. i wsp.: Quantification of tonic and phasic muscle activity in REM sleep behavior disorder. J. Clin. Neurophysiol., 2008, 25, 1, 48-55.
- de la Hoz-Aizpurua J.L. i wsp.: Sleep bruxism. Conceptual review and update. Med. Oral Patol. Oral Cir. Bucal., 2011, 16, 2, e231-e238.
- Castroflorio T. i wsp.: Detection of sleep bruxism: comparison between an electromyographic and electrocardiographic portable holter and polysomnography. J. Oral Rehabilit., 2014, 41, 3, 163-169.
- Deregibus A. i wsp.: Reliability of a portable device for the detection of sleep bruxism. Clin. Oral Investig., 2014, 18, 8, 2037-2043.
- Andrea B.: Validità di dispositivo portatile per la diagnosi di bruxismo nel sonno: confronto con esame polisonnografico. – Master Thesis. Università di Torino, 2011-2012.
- Castroflorio T. i wsp.: Use of electromyographic and electrocardiographic signals to detect sleep bruxism episodes in a natural environment. IEEE J. Biomed. Health Inform., 2013, 17, 6, 994-1001.
- Castroflorio T. i wsp..: Agreement between clinical and portable EMG/ECG diagnosis of sleep bruxism. J Oral Rehabil., 2015, 42, 10, 759-764.
- Manfredini D. i wsp.: Diagnostic accuracy of portable instrumental devices to measure sleep bruxism: a systematic literature review of polysomnographic studies. J. Oral Rehabil., 2014, 41, 11, 836-842